The Current State of the Art in Orthognathic Surgery
Recent decades have seen great advancements in orthognathic surgery. From rudimentary techniques to highly specialized and refined procedures, significant improvements provide improved function and aesthetics for patients with dentofacial deformities.
Innovation, collaboration, and a much deeper understanding of facial anatomy dominate today’s orthognathic landscape. Dr. Michael Stosich explores the four key components that make up today’s orthognathic landscape.
- Key surgical techniques
- The integration of new technologies
- Patient outcomes
- Ethical considerations.
1. What is Orthognathic Surgery?
Commonly referred to as jaw surgery, orthognathic surgery is a specialized surgical field that focuses on correcting jaw and facial skeleton abnormalities. Abnormalities can be congenital, meaning present at birth, or developmental, meaning they emerge over time. They can also be caused by trauma.
Orthognathic surgery’s primary goal is to realign the jaw. Once this is achieved, patients will see improved occlusion (how the teeth fit together), restored facial balance, and an enhanced quality of life. Surgery can also result in improved facial appearance, which can greatly enhance a patient’s self-esteem and emotional well-being.
An additional benefit of orthognathic surgery is improvement in appearance, which can significantly boost a patient’s self-esteem and emotional well-being.
There are many reasons why a patient may choose orthognathic surgery, including:
- Improve function. Patients may experience difficulty chewing, speaking, or breathing due to jaw misalignment.
- Improve aesthetics. Jaw abnormalities can cause facial asymmetry.
- Correct congenital deformities. Orthognathic surgery can correct issues such as cleft lip or palate, as well as other craniofacial issues.
- Correct trauma. Accident or injury can lead to skeletal deformities that require surgery to correct.
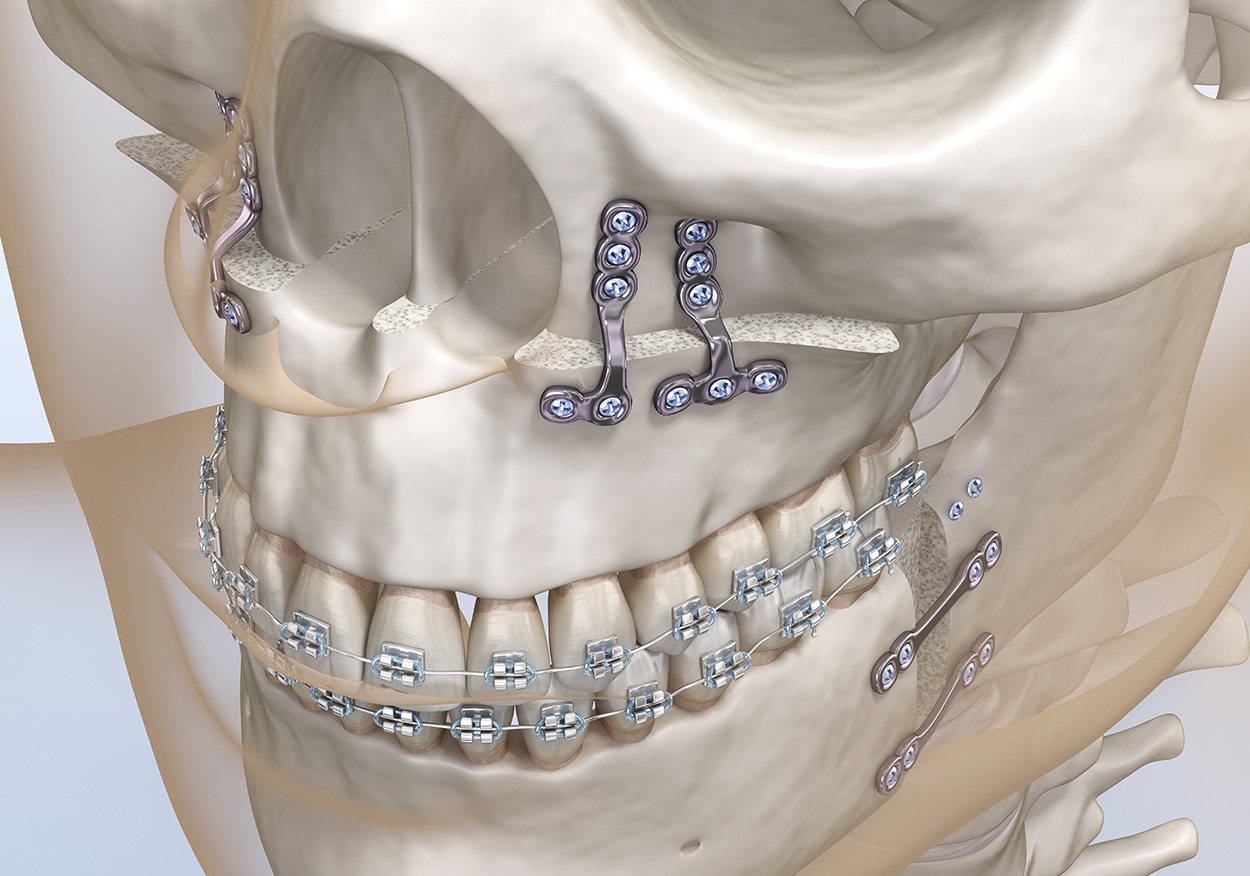
Comprehensive orthodontic treatment typically accompanies orthognathic surgery, both before and after. Treatment before can achieve a stable and functional bite, while treatment after can fine-tune the bite and stabilize the jaw.
2. Innovations in Orthognathic Surgery
Technology grows in leaps and bounds every day, and the orthognathic world is no different. Significant advancements have improved the precision and safety of jaw surgery.
- Virtual Surgical Planning (VSP) and 3D Imaging
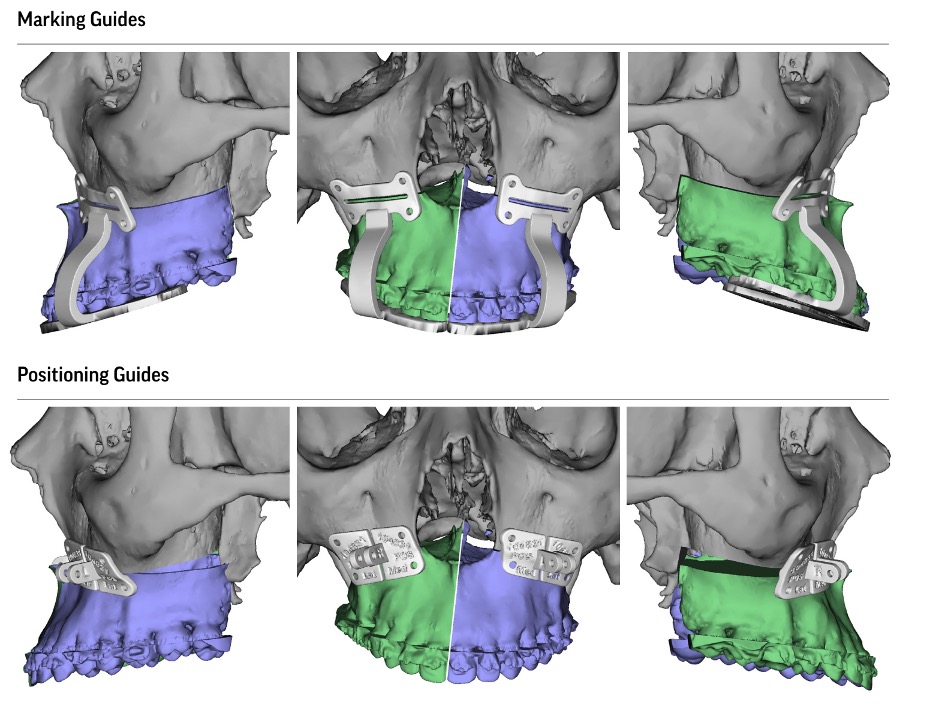
These tools allow surgeons to create detailed models of a patient’s facial skeleton before performing any procedure. This allows a surgeon to plan with astonishing precision and reduces the risk of complications and ensures optimal alignment. Combining virtual planning tools and 3-D printed surgical guides increases surgical accuracy even further.
- Minimally Invasive Techniques
Traditional orthognathic surgeries require extensive incisions and recovery periods. Newer minimally invasive techniques are changing that, however. These techniques focus on smaller incisions, reduced trauma to surrounding tissues, and quicker recovery times. This then helps us reduce potential complications and can even enhance the surgical outcome.
- Robotic-Assisted Surgery
Robotic technology is used in numerous surgical procedures, and we are now beginning to see them in orthognathic surgery, as well. This technology allows for more precise control in delicate jaw surgeries.
Robotic systems assist with bone cutting and realignment, ensuring greater consistency and reproducibility. While it is still in the early stages, we can expect robotic surgery to soon be a staple in the future of orthognathic surgery.
3. Surgical Techniques in Orthognathic Surgery
There are several surgical techniques available to address the different types of skeletal issues and deformities patients may present with. Each technique is tailored to the needs of the individual patient, some may be combined to achieve the best results. Surgical techniques include:
- Bilateral Sagittal Split Osteotomy (BSSO)
This is one of the most commonly performed to correct issues when the lower jaw protrudes too much. The surgeon will cut the mandile bilaterally, usually along the sagittal plane. Then, the jaw alignment can be corrected. This procedure is quite versatile and can address a wide range of deformities, from mild asymmetry to more significant issues such as prognathism or retrognathism.
The precision of BSSO procedures is enhanced with the use of 3D-printed surgical guides. Studies have shown that using these guides reduces the likelihood of surgical error, which can then lead to improved functional and aesthetic outcomes and faster recovery times. (Zhao et al., 2015).
- Le Fort I Osteotomy
This procedure is used to address issues where the upper jaw is underdeveloped. This is referred to as maxillary hypoplasia. The surgeon will cut through the maxilla, separating it from the rest of the skull. It is then repositioned forward, which corrects the bite and improves the facial profile.
Le Fort 1 osteotomy can be very effective for patients with class III malocclusions and those with retrognathic maxillae. Surgeons can also combine it with BSSO or other procedures to improve function and aesthetics. Modern innovations, such as virtual surgical planning (VSP), have increased the accuracy and predictability of this procedure, resulting in better overall outcomes (Zhou et al., 2019).
- Le Fort II Osteotomy (Pyramidal Osteotomy)
This type of surgery, also known as pyramidal osteotomy, treats milder deformities that affect the upper jaw and its associated facial features. This involves a more extensive separation of the upper jaw and the midface than the Le Fort 1 osteotomy. When performing this procedure, the surgeon is essentially “picking up” the entire maxilla to reposition it. This includes repositioning the nasal and orbital bones, as well.
This can be used in cases of midfacial hypoplasia or cleft lip and palate because it addresses more complex deformities, including congenital issues such as those from Treacher Collins Syndrome. Le Fort II can improve occlusion as well as correct aesthetic issues related to eye and nasal areas.
Le Fort Osteotomy II is a more complex procedure than Le Fort I, requiring a multi-disciplinary team. When an orthodontist and maxillofacial surgeon work together, we can achieve optimal results. Virtual surgical planning has made this procedure even safer and more predictable, thereby improving patient outcomes.
- Le Fort III Osteotomy (Craniofacial Osteotomy)
Also known as a craniofacial osteotomy, this procedure is the most extensive of the Le Fort surgeries. We use this to address the most severe midfacial deformities where bot the maxilla and entire midface are displaced. This procedure can be used for patients with syndromes such as Crouzon’s or Apert.
For this technique, the surgeon separates the entire maxilla and facial skeleton from the rest of the skull. This includes the orbits, nasal bones, and upper jaw. The midface can then be repositioned to correct functional and aesthetic concerns.
This procedure is performed on patients who have a recessed or malformed midface. It can correct severely retruded maxillas, significant facial asymmetry, or the inability to achieve facial balance through less invasive techniques. It can be combined with other procedures to ensure ideal facial balance and jaw function.
This is an incredibly complex procedure that requires careful planning and precise execution. This has made virtual planning guides and 3D models indispensable tools for this procedure, improving both technical execution and post-operative results.
4. Conclusion on Surgical Techniques
Advancements in orthognathic surgery have made it more effective than ever to treat severe skeletal deformities. The refinement of these now commonly used procedures has led to better results for patients, including improved facial aesthetics and restoration of essential functions, such as chewing, speaking, and breathing.
Le Fort II and le Fort III osteotomies are a significant step forward in the treatment of the most complex craniofacial abnormalities. They allow for the correction of midfacial and skeletal issues that were once too difficult to address. Advances in imaging and the use of virtual surgical planning have made these complex surgical procedures more predictable and precise. The continued and expanded use of these technologies will only continue to improve patient outcomes, offering life-changing results.
No matter the type or severity of the case, successful orthognathic surgery relies on a well-coordinated multi-disciplinary approach. Combining the skills and knowledge of an orthodontist and maxillofacial surgeon working together results in the best outcomes. Regenerative medicine, ongoing research in minimally invasive techniques, and AI-driven planning make the future of orthognathic surgery very bright. And that means enhanced precision, safety, and success for patients undergoing these transformative procedures.
References
- Zhao, Y., et al. (2015). “Multidisciplinary management of dentofacial deformities: Role of orthodontics and orthognathic surgery.” Journal of Oral and Maxillofacial Surgery, 73(5), 1019-1026. https://doi.org/10.1016/j.joms.2015.01.014
- Zhou, Y., et al. (2019). “Surgical advances in Le Fort I osteotomy: Improving outcomes and minimizing complications.” PubMed Central, PMC, 423-428. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6781234/
- Tatum, S. L., et al. (2016). “Le Fort II osteotomy in midfacial deformities: A comprehensive review and update.” Journal of Craniofacial Surgery, 27(4), 993-999. https://doi.org/10.1097/SCS.0000000000002751
- Singh, G., et al. (2020). “Advancements in Le Fort III osteotomy for craniofacial syndromes.” Journal of Craniofacial Surgery, 31(7), 1843-1850. https://doi.org/10.1097/SCS.0000000000006519